Better Community Care Through Collaboration
Adirondacks ACO, or “ADKs ACO,” is an Accountable Care Organization, a partnership of health care professionals that care for people in the Adirondacks and northern New York State.
At the ACO, we are a provider-led entity that is working together to create the future we all want, with high-quality care, improved efficiency and outcomes, lower costs of care, and increased patient and provider satisfaction. Our vision for the future is a system that allows providers to spend time seeing and helping patients. We partner with health insurance companies, hospitals, independent medical practices, and the community to help ensure that patients get the care they need when they need it at the lowest possible cost overall. We provide our network partners, such as doctors and other providers, access to data, resources, and tools to improve patient health and ultimately lower the cost.
Together, our goal is to make our community healthier and stay healthier by focusing on managing chronic illnesses and improving access to primary care and behavioral health services in New York.
AIM of
Adirondacks ACO
Adirondacks ACO will continue to focus on areas that ultimately support achieving high-value health care delivery in our region in 2023.
We do want to take a moment to reflect on our successes for 2022.
Adirondacks ACO will continue to focus on impacting these areas to achieve high-value health care delivery in our region in 2022
Provide our Network Partners with support that impacts care delivery
Boost the Overall Patient Experience

Improve the Health of our Communities
A Message From Our CEO, Eric Burton

Eric Burton
Interim Chief Executive Officer Adirondacks ACO
Chief Executive Officer Adirondack Health Institute
The healthcare industry has continued to face significant challenges over the past year. Unprecedented workforce shortages and fiscal pressures coupled with ongoing impacts of the global pandemic consume our partner organizations. We are grateful for the heroic efforts taking place on a daily basis to serve the communities that we live and work in.
Aside from these challenges, the regional participants for a second consecutive year in performance year 2021 earned more than three million dollars of shared savings in the Medicare Shared Savings Program. We are honored to work with such outstanding organizations who were able to produce these results in such demanding times. The Adirondack region continues to serve as a model for collaborative approaches to the value-based payment journey. Completion of our first full year of the affiliation between the Adirondacks ACO and Adirondack Health Institute and the second year of the North Country Care Coordination Collaborative are perfect examples of the collaborative spirit in the region.
A special thanks to our dedicated team and Board of Managers who make everything possible. We look forward to continuing to serve the region in the pursuit of building healthy communities and a sustainable rural health care system.
OUR NETWORK CONSISTS OF
5 HOSPITALS
53 PRIMARY CARE PRACTICES
8 PEDIATRICS PRACTICES
1,027
PROVIDERS IN THE ACO NETWORK
24
TOTAL NUMBER OF ORGANIZATIONS IN THE ACO

7
COUNTIES SERVED
Clinton, Essex, Franklin, Hamilton, Warren, Washington, and Northern Saratoga Counties of New York

8
PAYER PROGRAMS IN THE ACO
Medicare, Fidelis Medicaid Managed Care, Excellus, Empire BlueCross Blue Shield, Highmark, MVP, UnitedHealthcare -The Empire Plan, and BCBS VT
140,907
UPSTATE NEW YORKERS ARE COVERED BY PAYERS IN ACO PROGRAMS

39
MEDICAL SPECIALTIES WHO PARTICIPATE IN THE ACO
From Primary Care to Cardiology, Cancer Care and beyond!
Adirondacks ACO Results
Even with a global pandemic, Adirondacks ACOs network continued to achieve goals that support high quality care for our communities.
Shared Savings
The goal of the Adirondacks ACO Model is to support our partner organizations as we move the health care delivery system from what we know as volume-based to value-based payments. Our network providers have the opportunity to maintain their independence while having the value of shared resources, data, and supports that will better prepare them for this shift in health care delivery. Providers have the opportunity to achieve shared savings when collectively we meet financial and quality goals that benefit the community as a whole. This way, we can ensure that patients, especially our most vulnerable community members with complicated health issues, have the supports needed and our network providers have the resources to do what is needed to make a difference in the community.
The Adirondacks ACO earned $3.4M in shared savings, reflecting two consecutive years of shared savings for the region’s providers. Congratulations and great work to all in achieving this milestone.
Comparing 2020 financial performance with 2021 –
Total savings: $8,628,669 in 2021, improved from $7,879,019 in 2020.
Eligible Shared Savings: $3,382,438.08 in 2021, improved from $3,062,968 in 2020.
According to the National Association of ACOs (NAACOS), overall the Medicare Shared Savings Program ACO model served 11 million seniors in 2021 and collectively achieved $3.6 billion in gross Medicare savings, and $1.6 billion after accounting for shared savings payments. Of the 475 MSSP ACOs, 81% achieved Medicare savings with 56% earning actual shared savings. Nearly all ACOs – 99% – reported and met the quality standard required to share in savings under the Shared Savings Program.
In 2021, we did earn an additional $575,000 in shared savings with four of our six commerical health plan partners, however this was less than 2020. While our Managed Medicaid value-based payment contract did not earn any shared savings, we also did not experience any loss.
It is important to note that our 2021 expenditures benchmarked to our 2020 experience determines the shared savings/shared losses. The impact of the pandemic on overall utilization in 2020 could be a contributing factor compared to our overall performance in 2021.
In early November 2022, we were able to distribute $3.6 million dollars to our participating partner organizations, representing 99% of the savings earned with the 1% balance utilized to offset participant fees that support the ACO infrastructure.
“The work of the Adirondack Accountable Care Organization is moving along steadily. We are exploring the potential of our new and enhanced data analysis capabilities; we continue to do very well with quality measures, and we continue to enhance cooperation among our partner providers. We have been anticipating the onset of the New York State 1115 waiver and evaluating what we will need to do to meet the challenges of this large initiative. All of our members struggle in some fashion with the large and rapid changes in the health care world and we are committed to assisting in setting common goals and keeping focused on providing reliable excellent patient centered care.”
2021 Quality Snapshot
The pandemic of 2020 presented many challenges for our network providers, patients, and communities. These challenges impacted the healthcare community and how they delivered care. Practices quickly adapted to delivering care via telehealth, to ensure patients were getting their personal health needs met without putting them at risk.
The switch in how our Network provided care created workflow challenges and changes from billing, connectivity, and staffing challenges to name a few. As practices worked through these challenges, our Network successfully submitted and maintained our NYS PCMH recognition, along with increasing quality performance across the Network.
The Medicare Shared Savings Program total quality score for 2021 was 91.06%, which allowed the ACO to earn the full 40% of eligible shared savings. Overall, the ACO made improvements in six out of ten quality measures – screening for fall risk, depression screening, colorectal cancer screening, breast cancer screening, diabetes – poor control, and hypertension. Slight declines in performance were reported for influenza vaccination, tobacco use and cessation intervention, statin therapy for preventative cardiovascular disease, and depression remission at twelve months.
The ACO patient experience scores were above the mean performance rate for all Medicare Shared Savings Programs for seven of the ten defined areas, with significantly higher performance for communication, health promotion and education, care coordination, courteous and helpful office staff, and overall provider rating.
The quality score for our commercial contracts is a blended score of thirteen measures across six health plans, based on both claims data and clinical data. Three of the thirteen measures rely on manually abstracted data from the charts of a random sample of patients who receive care in our provider network. In 2021 we saw a 38% increase in our overall global score – increasing from 46.15% in 2020 to 64.10% in 2021. We saw an increase in scores for breast cancer screening, colorectal screening, child and adolescent immunizations, well child visits for children age 15-30 months, controlling hypertension, diabetes poor control management and depression screening.
2022 Quality Highlights
At Adirondacks ACO, we have continued on our positive trajectory for 2022.
Although our Network has faced obstacles, we have collectively worked with our Network to ensure we can continue to see positive outcomes.
Our approach to establishing 2022 performance year (PY 2022) benchmarks utilizes the NYS QARR data published for 2020. This data is a compilation of our plan partner data measured at the 50th, 75th and 90th percentile for each quality measure – earning incremental points for each percentile we achieve. This method of approaching an overall quality score provides credit for marked improvements compared to existing plan data.
Early trends show that the results for three quality measures will likely score lower than expected for PY 2022. To note, controlling hypertension, depression screening and depression remission at 12 months may require a more focused approach that is more consistent with the measure specifications and required clinical documentation.
Early trends also show that the management of poorly controlled diabetics showed marked improvement from prior performance periods. Based on a statistical sample of diagnosed diabetics, the majority regularly had their A1C monitored, with the majority of the test results at less than 9%, the gold star of good diabetes management.

According to the World Health Organization (WHO) undermanaged diabetes can damage the heart, blood vessels, eyes, kidneys and nervous system – all contributing to poor health outcomes and increased health care costs. The 2021 ACO data across all health plans identified 17,306 individuals with a diagnosis of diabetes and 10,696 with a diagnosis of prediabetes.
In early 2022, the ACO Team embarked on a journey to focus on prevention and treatment of prediabetes and diabetes. Each identified area plays a role in both prevention, appropriate treatment and adequate support resources.

Adirondacks ACO worked with network providers to assess their ability and readiness to move to electronic clinical quality measurement (eCQMs), as CMS Medicare Shared Savings Program will require the quality submission to be via eCQMs for measurement year 2025. Participating provider groups made consistent efforts to submit data to the ACO Data Team based on the eCQM criteria, however some groups continue to experience on-going issues that limit their ability to successfully report for their patient panel. Despite these challenges, this will continue to be a significant focus in 2023 to ensure we are prepared to report as early as 2024.
Adirondacks ACO Partner Collaboration Programs
When working as an ACO, our care goals become apparent when we work together with our network providers and community members.
“The QUIC dashboard report is ‘an eye opener’. When you see a population list and see some of the accounting for PPEs and individuals with high numbers, there is a lot of value in that.”
Partner Program:
Behavioral Health Services North (BHSN)

Behavioral Health Services North (BHSN) has been very successful over the last few years in achieving positive outcomes not only for their clients, but also for their own organization and the Northwinds IPA as a whole. Shawn Sabella, VP of Strategy, Quality, and Government Relations, takes full advantage of the reporting, workgroups, and support offered by both the IPA and the ACO. Shawn noted that attending the various workgroups has provided him a forum to ask questions where they could seek answers from other behavioral health and substance use organizations facing similar challenges. If he misses a workgroup, he is sure to reach out and ask for the materials shared to stay on top of what is going on in the community.
Shawn takes the time to dive deep into the data sources that BHSN has available to them – whether that be the ACO Quality, Utilization, and Integrated Care (QUIC) dashboard, Hixny, PSYCKES, or their own EMR.
Shawn finds the QUIC dashboard especially helpful when reviewing BHSN’s performance on medically focused measures such as colorectal and breast cancer screenings, or postpartum care – this information is not readily available in other data sources. He also noted that the QUIC dashboard is helpful when drilling down to a specific client and reviewing quality flags, and most importantly, reviewing the Potentially Preventable Events (PPE) report. He said this report is “an eye opener – when you see a population list and see some of the accounting for PPEs and individuals with high numbers, there is a lot of value in that.”
When it comes to care management and working with clients in the community, Shawn shared that Mary Baker, VP of Care Management Services, has “been an anchor at BHSN for over 25 years”. Both Mary and Shawn regularly attend the North Country Care Coordination Collaborative (NCCCC) meetings and are appreciative of the effort made by this group to try and make improvements around the care management workforce, especially when the job demands are very rigorous, and recruitment/retention is a challenge. BHSN’s care management team has had success this past year in connecting people to primary care. Their care managers help clients connect to necessary services after an inpatient stay, make sure they have their medications, connect them to community resources such as housing, and so much more.
Partner Program:
Glens Falls Hospital

Ann Marie Hatch, Senior Director of Physician Practices shared that one of the wisest things the hospital did was create a centralized team for primary care that schedules calls, triages, handles e-scripts, and all referrals. Since this centralization occurred, their internal referral rate has improved almost 40% – a critical move when looking at care coordination, less redundancy and duplicative testing, and cost control.
An additional component to their centralization team is a smaller group of individuals who focus on gaps in care. This team handles pre-visit planning, reviewing patient records, and looking at all gaps in care reports – from both payers and the ACO. The team places important notes on the appointment line so the care team and provider can see what is missing in an effort to provide appropriate care. ACO and payer reports allow them to ensure they focus on the right patients. In 2023, the hospital will have more staff available to review these reports with one person focusing on patients who need colorectal screenings, one person focusing on breast cancer screenings, etc.
When it comes to care management, Glens Falls Hospital has been an active participant in the North Country Care Coordination Collaborative (NCCCC). Recent trainings put on by the NCCCC have been invaluable for their care managers. Jolynn Pierce, Program Manager, shared some recent changes they have made to their care management team. An important add has been employing transitions of care (ToC) coordinators who handle all calls to patients coming out of the ED and inpatient for all sites. The hospital’s care management team also recently started combining RN embedded care managers with their Health Home care coordinators out in the community to wraparound high acuity patients.
A positive outcome of this approach involved a patient who was not as engaged as was desired with primary care visits, not managing their medications, frequently admitted to the hospital, and was at risk of losing their primary care due to a lack of engagement. The RN care manager and health home care coordinator worked together alongside the patient, helping them to secure an alternate level of living. Over the course of a few months, the patient is now in assisted living, makes all of their appointments, takes all medications as prescribed, and has had zero admissions to the hospital since implementing this team approach.
Adirondacks ACO
Network Participants
Adirondacks ACO is an Accountable Care Organization (or ACO) made up of groups of doctors, hospitals, and other health care providers, who all work together to deliver high-quality, coordinated care.
Adirondacks ACO
Board Members
Adirondacks ACO is governed by a Board of Managers that provides oversight of the services needed to fulfill the Quadruple Aim: “Improve the Quality of Care, Increase Patient Satisfaction, Lower the Cost of Care, and Increase Provider Satisfaction.”
Adirondacks ACO’s Board of Manager’s includes providers from all sectors of our regional health care system, as well as local residents who represent Medicare and Medicaid beneficiaries, and an individual who advocates for the uninsured. These individuals actively participate in board meetings, provide community input and guidance, and vote on all matters that come before the board.
Adirondacks ACO 2023 : Minimizing The Impact
Our provider network partners continue to feel the impact of the pandemic amidst unprecedented workforce challenges. Our focus for 2023 will be to continue to minimize the downside risk with our payer contracts, while maintaining current levels of financial support. Our enhanced data capabilities will focus on tools that support partner priorities, ultimately enhancing patient health outcomes, both leading to improved value based payment performance.
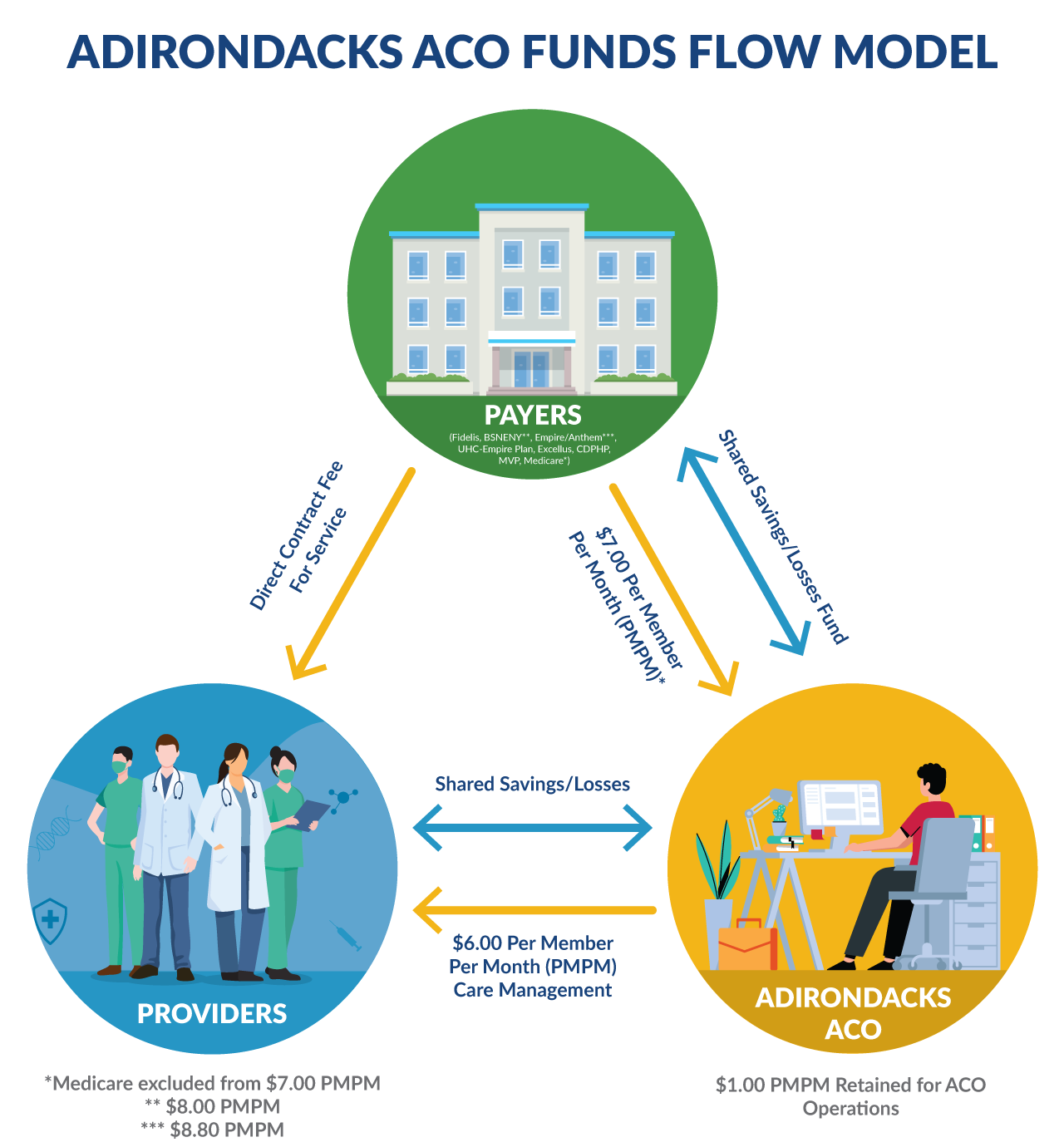
Financial: Adirondacks ACO Funds Flow
The Adirondacks ACO continues to ensure that the Per Member Per Month (PMPM) funds flow to our participating primary care providers on behalf of our payer partners. The ACO administrative costs continue to be carefully monitored to ensure that only a fraction of the total PMPM is needed to support our infrastructure.
2022 Contracting Strategy - Stay The Course
ACO Leadership conciously decided to approach 2023 contracting with a “stay the course” theme and minimize any additional burden to our network providers. We approached each health plan wiht the intent to maintain their 2022 contract with the same expectationsand shared savings/risk parameters as we had in 2021. This approach would also include the continuation of the PMPM funds that were received in 2021 and in prior performance periods.
We were successful with our approach and with the exception of one plan, maintained our 2022 contract without additional risk to our participating partners. This strategy outlines our guding principles for 2022 with three focus aresa –

Financial
Maximize provider incentives while mitigating downside risk

Quality & Data
Align metrics and data reporting across all payers and reduce the administrative burden for each provider organization

Network & Community
Maximize attribution and expand support for Community Based Organizations that enhance our Mental Health and Substance Use Disorder/Primary Care Provider Integration
Adirondacks ACO Data and Performance Tools
State of ACO Data Analytics
2022 was a busy year for ACO data and data analytics. To start, our team welcomed a new team member, Amber Baker, and said a bittersweet farewell to Lilian Wu, all the while continuing to supply providers and partners with the reports and information they’ve come to expect and need. Our greatest achievements for this year include:
1. Client Data Warehouse (CDW) Implementation
The new CDW, a standalone data base containing ACO members’ payer claims information and Hixny health information exchange (HIE) clinical information, was successfully built with the HIE data fully connected and the largest payers’ claims data fully integrated Adirondacks ACO Data and Performance Tools. As you can see from the accompanying implementation timeline, the data team, with the help of Hixny, has now begun moving into the next phase of project, which is leveraging this new, more comprehensive data source for reporting.
Implementation Timeline
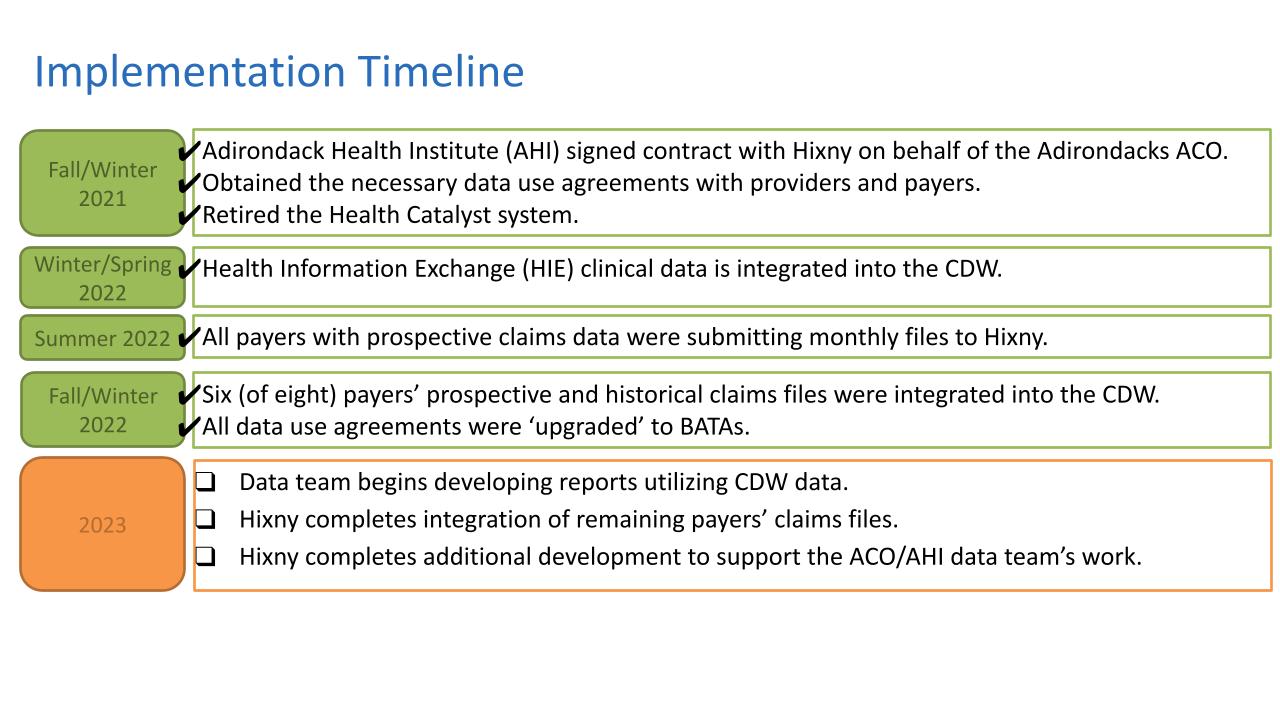
Winter/Spring 2022
- Health Information Exchange (HIE) clinical data is integrated into the CDW.
Summer 2022
- All payers with prospective claims data were submitting monthly files to Hixny.
Fall 2022
- All payers with prospective claims data were submitting monthly files to Hixny.
- Four (of six) payers’ prospective and historical claims files were integrated into the CDW.
Ongoing
- Data team is starting to develop reports inclusive of CDW data.
- Hixny is working on integrating remaining payers’ claims files.
- Hixny is engaged in additional development to support data team’s work.
2. Electronic Clinical Quality Measures (eCQM) Reporting
The Adirondacks ACO and Adirondack Health Institute have continued to prepare for ACO reporting of CMS’ electronic clinical quality measures (eCQMs). The ACO’s Quality and Data staff has been working closely with the ACO providers and their electronic health record (EHR) vendors to obtain the reports necessary for the ACO to successfully complete this reporting. Additionally, the data analytics team has successfully built the capability to process the various EHR-generated files and generate ACO-level results for submitting to CMS. Performance year (PY) 2022 will be a transition year towards sole eCQM reporting in that the ACO intends to submit measure results using both the eCQM methodology as well as the ‘traditional’ web interface methodology, with the expectation that only eCQMs will be reported for PY 2023. Once implemented, this capability will free up valuable time for clinicians/support staff and let our partners focus on patient care.

3. New and Updated Data Reporting
Several new, as well as, refreshed reports were distributed to the ACO providers in 2022. These include the Wellness Visit Report, the Social Determinants of Health Report, the Care Navigator Report, and the Gaps in Care Reports. A summary of these reports and their uses is provided in the accompanying report grid. In addition to these reports, we also began distributing a Quality, Utilization, and Integrated Care (QUIC) interactive dashboard to our Northwinds IPA partner providers. Report Spotlights:
- The Revised Gaps in Care Reports
The first new feature of the Gaps in Care Report is that it was divided into two separate reports:
1) the Primary Gaps List Report, containing three high priority screening visit measures with gaps, and 2) the Secondary Gaps List Report, containing the remaining measures with gaps.An additional new feature is that the Primary Gaps List Report also includes Hixny Health Information Exchange (HIE) information about patients’ qualifying screening visits conducted by any provider participating in the Hixny HIE, including screening date and provider.The purpose of these two reports is to support ACO providers’ ability to 1) Clinically address gaps in care, and subsequently increase quality scores, by providing a working list to assist ACO providers with identifying, scheduling, completing, and/or documenting missing healthcare services; and 2) Inform supplemental data submission for payers and measures accepting documentation of closed gaps. - The New Quality, Utilization, and Integrated Care (QUIC) Dashboard
This interactive dashboard was developed for our Northwinds IPA partner providers to assist them in achieving the goals of their Medicaid Managed Care and HARP value-based contracts. The dashboard includes 11 quality measures that are updated quarterly. This dashboard was built with the network in mind – creating a common framework for quality improvement, focusing on common measures, providing performance and improvement accountability, and supporting a more complete view of provider capacity and risk to inform contract negotiations.

Citizenship Criteria: For 2022 Performance Year
2021 was the first year that the Board of Managers agreed to apply the citizenship criteria adherence to participating provider shared savings and losses.
2021
Citizenship Summary
- 80% of all ACO providers achieved a score of 100% across all criteria (8 total points).
- All ACO providers achieved at least a score of 75% (6 out of 8 total points) with engagement criteria being the lowest (92% achieved).
- 100% of all ACO providers met the citizenship criteria for care coordination (use of risk stratification or risk coding initiative).
- 67% of all Northwinds providers achieved a score of 100% across all criteria (8 total points).
- Northwinds providers scored highest on quality criteria (89% achieved) but scored lower on care coordination and engagement (44% criteria achieved).
2022
Citizenship Summary Preview
- 80% of all ACO providers achieved a score of 100% across all criteria (8 total points) – this is the same as 2021.
- ACO providers scored highest on quality criteria (95% of points earned).
- 91.7% of all Northwinds providers achieved a score of 100% across all criteria (8 total points) – this is an almost 25% increase from 2021!
- NWIHN providers scored 100% on both quality and care coordination criteria.
Adirondacks ACO Staff
“Within our ACO team and throughout all of our partner organizations, I am honored to be working alongside such talented, compassionate, and professional individuals. The client focused work as well as the behind the scenes work happening to improve the health and wellbeing of the Adirondack region is incredible.”

Melissa Joyce
Support Specialist II
Adirondacks ACO

Eric Burton
Interim Chief Executive Officer (CEO)

Karen Ashline
Vice President

Wouter J. Rietsema, M.D.
Chief Medical Officer

Justin Frazer
Compliance Officer

Katy Cook
Director of Partner Engagement

Jeremy Powers
Director of Clinical Quality Improvement and Practice Transformation

Laura Morris
Director of Data Analytics

Lisa Cyphers
Senior Performance Improvement Analyst

Melissa Joyce
Support Specialist

Tyler Babbie
Accountant

Karlee Strong

Kate Pabst

Amber Baker
Support Specialist
Adirondacks ACO
Insurance Plans
Adirondacks ACO serves as the provider network for government-sponsored and commercial insurance plans called “payers” that are available to New York residents. By partnering with an ACO like us, government and commercial payers can offer affordable insurance products where the provider network is motivated to deliver quality care at a lower cost, which benefits the patient, the payer, and the provider.
