Better Community Care Through Collaboration
At the ACO, we are a provider-led entity that is working together to create the future we all want, with high-quality care, improved efficiency and outcomes, lower costs of care, and increased patient and provider satisfaction. Our vision for the future is a system that allows providers to spend time seeing and helping patients. We partner with health insurance companies, hospitals, independent medical practices, and the community to help ensure that patients get the care they need when they need it at the lowest possible cost overall. We provide our network partners, such as doctors and other providers, access to data, resources, and tools to improve patient health and ultimately lower the cost.
Together, our goal is to make our community healthier and stay healthier by focusing on managing chronic illnesses and improving access to primary care and behavioral health services in New York.
AIM of
Adirondacks ACO
We strive to ease the administrative burdens by providing our network partners access to data, resources, and tools to improve patient health in our area.
Adirondacks ACO will continue to focus on impacting these areas to achieve high-value health care delivery in our region in 2024
Provide our Network Partners with support that impacts care delivery
Boost the Overall Patient Experience

Improve the Health of our Communities
A Message From Our CEO, Karen Ashline

Karen Ashline
Chief Executive Officer Adirondacks ACO
Chief Executive Officer Adirondack Health Institute
The unprecedented workforce shortages and fiscal pressures continued to be a significant issue our regional partners faced in 2023. Despite these challenges, we – as well as our families, friends, neighbors, and community members – continued to have access to the region’s partner supports and services that shape and touch our daily lives.
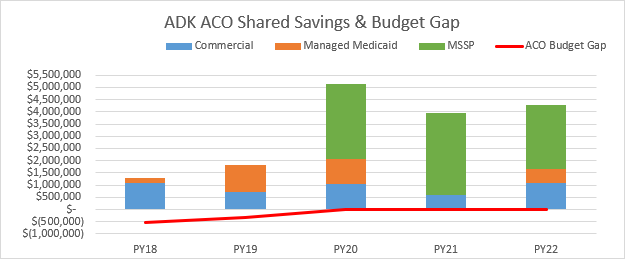
As our healthcare partners continued to try to recover from the economic and workforce challenges heightened by the pandemic, our participating ACO partners earned over $2.6 million of shared savings in the Medicare Shared Savings Program. This coupled with shared savings from our commercial health plan partners and Managed Medicaid provided a total of $4,268,947.12 shared savings and quality incentive dollars – all directly passed on to our participating partners.
This is the third consecutive year that 100% of the total shared savings were distributed to our partners. The ACO budget gap has significantly diminished with the shared AHI/ACO operational team. We are honored to work with such outstanding organizations who were able to produce these results in such demanding times. The Adirondack region continues to serve as a model for collaborative approaches to the value-based payment journey.
I was honored to be appointed CEO effective 1/1/2024 – taking a role that is an evolution of the work I have done since the inception of the Adirondack Medical Home Pilot in 2009. I am excited to lead our work, providing our regional partners with the resources needed to enhance the care we all deserve.
A special thanks to our dedicated team of staff and the ACO Board of Managers who make everything possible.
We look forward to continuing to serve the region in the pursuit of building healthy communities and a sustainable rural health care system. A special note of thanks to Eric Burton who served as the shared CEO for AHI and the Adirondacks ACO from September 2020 through December 2023 – his presence will be missed.
OUR NETWORK CONSISTS OF
5 HOSPITALS
51 PRIMARY CARE PRACTICES
9 PEDIATRICS PRACTICES
947
PROVIDERS IN THE ACO NETWORK
18
TOTAL NUMBER OF ORGANIZATIONS IN THE ACO

7
COUNTIES SERVED
Clinton, Essex, Franklin, Hamilton, Warren, Washington, and Northern Saratoga Counties of New York

8
PAYER PROGRAMS IN THE ACO
Medicare, Fidelis Medicaid Managed Care, Excellus, Empire BlueCross Blue Shield, Highmark, MVP, UnitedHealthcare – The Empire Plan, and BCBS VT
125,000+
UPSTATE NEW YORKERS ARE COVERED BY PAYERS IN ACO PROGRAMS

47
MEDICAL SPECIALTIES WHO PARTICIPATE IN THE ACO
From Primary Care to Cardiology, Cancer Care and beyond!
Adirondacks ACO Results
Despite the unprecedented challenges still felt as a result of the impacts of the pandemic, Adirondacks ACOs network continued to achieve goals that support high quality care for our communities.
Shared Savings
In 2022, the Adirondacks ACO earned $4,268,947.12 shared savings for the region’s providers, which is only $20,000 less than 2021. An achievement that is made possible by the dedication and commitment of our provider network.
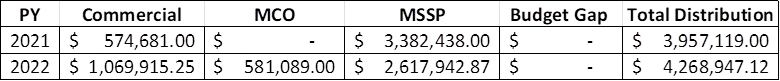
*2023 Results Not Available
2022 Quality Snapshot
2022 was another strong year for the ACO’s Medicare Share Savings Program (MSSP), finishing the year with a Final Score of 94.2% and a final shared saving total of $2.6 million. Diabetes Poor Control continued strong performance, falling to less than 12% of Medicare patients with an HbA1C greater than 9%. Breast Cancer Screening and Controlling Hypertension also continued with top performance. We also saw a 3% improvement in our Promoting Operability Performance, a testament to the continued advancements in EMR technology among our Primary Care Partners.
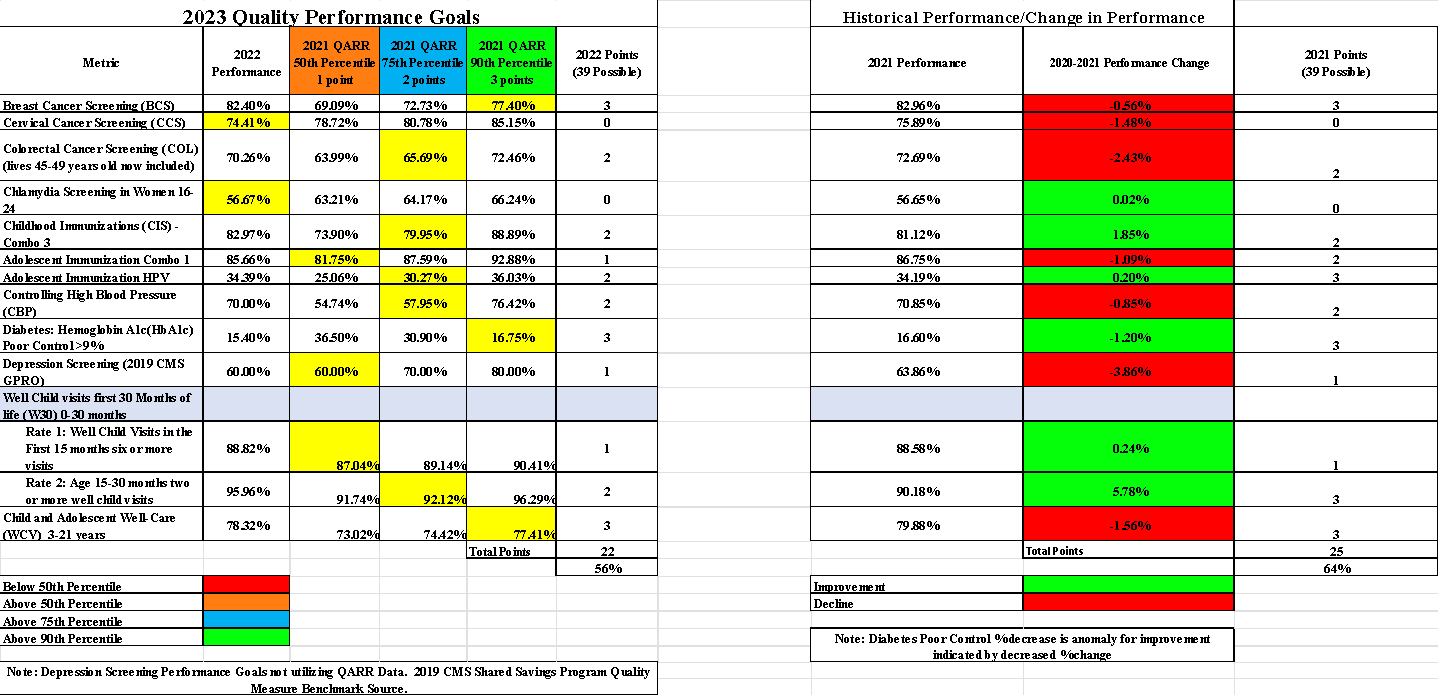
Along with the MSSP program, the commercial value-based-arrangements also showed continued improvement in Breast Cancer Screening and Diabetes Poor Control falling to less than 16% of commercial patients with an uncontrolled A1C above the 90th percentile. The final results demonstrated the success of our partners with 8 out of 13 measures on our global scorecard above the 75th percentile and another 3 above the 50th percentile! These results are especially impressive with complex measures included and several measures that were in their 1st year with formal benchmarks in place.
We are currently closing out the Manual Abstraction process with the Performance Year 2023 CMS submission complete. Preliminary results look very promising, extending improvement on the prior measures and showing improvement in 8/10 measures that contribute to the quality score. This improvement aligns with an increase in the weighted score as well demonstrating that the improvement outpaced our peers.
As we closed out the calendar year, we took a close look at the methodology for our global quality score that was directly connected to quality benchmark thresholds. In review, it was evident that there were some limitations to the prior methodology which did not capture performance progress between benchmarks and due to the point system, rounded to certain percentiles. We were able to gain approval from our MCO partners to make three positive changes to ensure our partners received credit for every bit of improvement they achieve.
Both the score between benchmarks and between points will be measured on a scale to capture the incremental improvement. In addition, we will be transitioning to HEDIS benchmarks from NYS QARR benchmarks. The HEDIS benchmarks, though national, are more homogenous with our population than the NYS QARR benchmarks that are more heavily influenced by the major cities. We feel that these changes will more accurately capture the hard work of our partners.
In 2023, the Diabetes Initiative, a workgroup under the Population Health Advisory Committee, reassessed the goals of the workgroup. In doing so, the group elected to simplify the goals as they had grown very diversified. The 3 new goals were to reduce the prevalence of diabetes in the region, improve health outcomes for those with diabetes, and to optimize and maximize ACO VBP opportunities pertaining to diabetes and prediabetes.
To build a foundation for the renewed work, the ACO Data Team developed a robust Diabetes Dashboard at the population health level.
The dashboard not only includes the diabetic population but also data available on the prediabetic. There are a host of key measures for these special populations as well as inclusion of ED and hospital utilization.
The new Chronic Disease Care Coordination Network is a project designed to improve access to evidence based Chronic Disease Self-Management Programs (CDSMP) and other social care programs. Improved health outcomes will be achieved through more effective case management/care coordination that facilitates referrals from clinical to social care providers for adults with heart disease and underlying conditions such as diabetes, hypertension, and heart diseases living in the four rural counties of Clinton, Essex, Franklin and Hamilton.
*Additional diabetes focused work includes the Adirondacks ACO partnering with the Adirondack Health Institute on a new HRSA grant focused on rural health care coordination.
Adirondacks ACO Partner Collaboration Programs
“The coordinated care and access to data and analytics have made CVFC more mindful, leading to improved patient outcomes. It truly feels like we are breaking down the barriers between physical health and behavioral health, perfectly complementing the CCBHC model.”
Jake Coulombe
CCBHC Director
Champlain Valley Family Center
Partner Program:
Champlain Valley Family Center (CVFC)

One of those measures includes time to service – from the first contact with an individual, how quickly are they getting someone engaged in screening and assessment. Another is post-assessment, time to clinical services being delivered. There is also a huge emphasis on screening instruments, whether it is a PHQ-9 regardless of presentation of a depressive disorder, and/or the CMS Accountable Health Communities instrument.
CVFC has already begun using this instrument which will be a key screening tool for the NYS 1115 Medicaid Waiver. They have established workflows and will ensure this is a part of every assessment for every patient, especially as a case management tool. CVFC also has some internal metrics that they wrote into the grant focused on dialectical behavior therapy, or DBT. Their prevention staff have been trained on the curriculum for DBT, and their clinicians are currently being trained on DBT Skills Step A (a 3-day training) with targets set for evidence-based practices that will be delivered. CVFC also intends to roll this curriculum out with summer programs in schools for kids at risk. They hope to work with between 50 and 60 kids. Their prevention coordinator said it is by far the best training she has ever attended and is already seeing the benefits.
Looking further into data, CVFC has contracted with a company called CCNY out of Buffalo – a not for profit data scientist company that will build a dashboard for the team that integrates with their EMR, pulling data into Power BI and automatically collecting information on all the CCBHC metrics. Other metrics they are looking at in the QUIC dashboard or PSYCKES include targeted case management. This is different from Health Home care management in that anyone can qualify but individuals will be worked with for a shorter time frame. CVFC has hired an RN dedicated to this process to build relationships with primary care providers, specifically Northwinds Primary Care and CVPH Family Medicine. Workflows have been established and agreements executed to ensure seamless referrals. Hiring an RN to speak with clinical teams at primary care offices has ensured successful collaboration, advocacy for service recipients, and whole-person care. Not only is a referral made, but they ensure the patient has transportation and will even sit with them at an appointment if they have social anxiety. This takes some of the work off the clinician’s plate and provides a dedicated focus to the PCP connection metrics.
CVFC has also implemented several initiatives focusing on specific populations, one being veterans. They are hoping to grow how many veterans they support, first by partnering with Valerie Ainsworth, Executive Director of the Mental Health Association of Essex County and their Homeward Bound Adirondacks Program which offers case management services, suicide prevention, wilderness retreats, transportation, homeless assistance, peer advocacy, crisis outreach, and more.
CVFC and Homeward Bound Adirondacks developed workflows around the services the program provides. They also started an advisory panel dedicated to veterans which consists of Board members, staff members, community members, and service recipients who are all veterans. The advisory panel has met once so far and plans to meet again on April 15th. The goals of this panel are to get CVFC out in the community and do some outreach to show veterans that this is a safe place to be. They have dollars to support veterans with treatment if needed, knowing insurance (Tricare and VA) can be a barrier to access.
To take this work a step further, CVFC has trained all their staff in cultural competency with the veteran population and are looking to hire veterans as peers on staff. Connie Wille, CEO of Champlain Valley Family Center said, “This is the most animated and emotional I have seen Jake in a long time after the advisory panel.” Jacob said this work “energizes me” and he hopes to reduce the stigma of seeking out mental health support in the veteran community.
Another important initiative that CVFC has embarked on is their Diversity, Equity, and Inclusion (DEI) Committee. This committee seeks to understand if certain populations are treated differently than others, such as an individual coming in with Medicaid who has been their multiple times versus a self-referred private insurance individual. By asking themselves the tough questions, they can place a greater emphasis on marginalized populations, especially individuals living in poverty or below the ALICE threshold. They’re also collecting outcome data to see if patients with private insurance have a higher rate of successful completion versus someone with Medicaid. They want to remain cognizant of the fact that data represents the people in the community, and they want to improve health outcomes for all.
Enrico Cullen, Executive Director for the Northwinds Integrated Health Network, says that CVFC “are premier partners for the IPA. The CCBHC status as an extension project is a major step forward in the integration of mental wellness and physical care in the North Country. This is a really big deal – people of the North Country will get better services, more integrated care, more holistic care, and this is simply better for the communities we serve.”
For more information, please contact Jacob Couloumbe, jcouloumbe@cvfamilycenter.org, or Connie Wille, cwille@cvfamilycenter.org.
Partner Program:
The University of Vermont Health Network
Alice Hyde Medical Center
Angela Bashaw, Director of Programs and Practice Support shared that the relationship with the Adirondacks Accountable Care Organization (ACO) and Adirondack Health Institute (AHI) began many years ago with the accreditation of their practices for Patient Centered Medical Home through NCQA. Angela notes that the support from the ACO through this transition into recognized PCMH practices was a “marked change in our journey into value-based care.”
She also shares, “Focusing on care gaps and quality metrics that are national standards, we have been very successful in achieving our goals which leads to better patient outcomes and care.” Consistent monitoring of these gaps in care has led to patient specific work and increased patient engagement. A significant amount of work has gone into the transition to a new EMR system and ensuring their data paints a good picture of the care being provided and is a good representation of how they are caring for patients, all while ensuring better health outcomes.
Angela shares that each primary care practice has a quarterly review of their quality metric performance, and they discuss where they may need to focus for the next quarter, ways of making improvements, patient outreach, etc. They make quality improvement plans at a practice level because even though they are a small rural community, the patient populations at each location can vary.
“By long-term, consistent tracking of our progress via data, we can see where we need to focus or where we may be falling in a timely manner. We can then focus on resources and workflows on supporting our patient population. Our Care Management (CM) team has been very helpful in this. We are grateful for them as they have provided care coordination, health home care management, and chronic disease patient education. Over the years, CMs have been a great resource and support in many ways from medical home to health home, and extra programs like diabetes education and tobacco treatment specialists are added support via shared savings.”
AHMC has been an active participant in the Chronic Disease Care Coordination Network (CDCCN), an AHI-led grant that continues the work of the North Country Care Coordination Collaborative (NCCCC). This continued partnership with not only the Adirondacks ACO but with AHI through the former DSRIP waiver, has changed the way they provide care.
Adirondacks ACO
Network Participants
Adirondacks ACO is an Accountable Care Organization (or ACO) made up of groups of doctors, hospitals, and other health care providers, who all work together to deliver high-quality, coordinated care.
Adirondacks ACO
Board Members
Adirondacks ACO is governed by a Board of Managers that provides oversight of the services needed to fulfill the Quadruple Aim: “Improve the Quality of Care, Increase Patient Satisfaction, Lower the Cost of Care, and Increase Provider Satisfaction.”
Adirondacks ACO’s Board of Manager’s includes providers from all sectors of our regional health care system, as well as local residents who represent Medicare and Medicaid beneficiaries, and an individual who advocates for the uninsured. These individuals actively participate in board meetings, provide community input and guidance, and vote on all matters that come before the board.
Adirondacks ACO 2024
Our provider network partners continue to feel the impact of the pandemic amidst unprecedented workforce challenges. Our focus for 2024 will be to continue to minimize the downside risk with our payer contracts, while maintaining current levels of financial support. Our enhanced data capabilities will focus on tools that support partner priorities, ultimately enhancing patient health outcomes, both leading to improved value based payment performance.
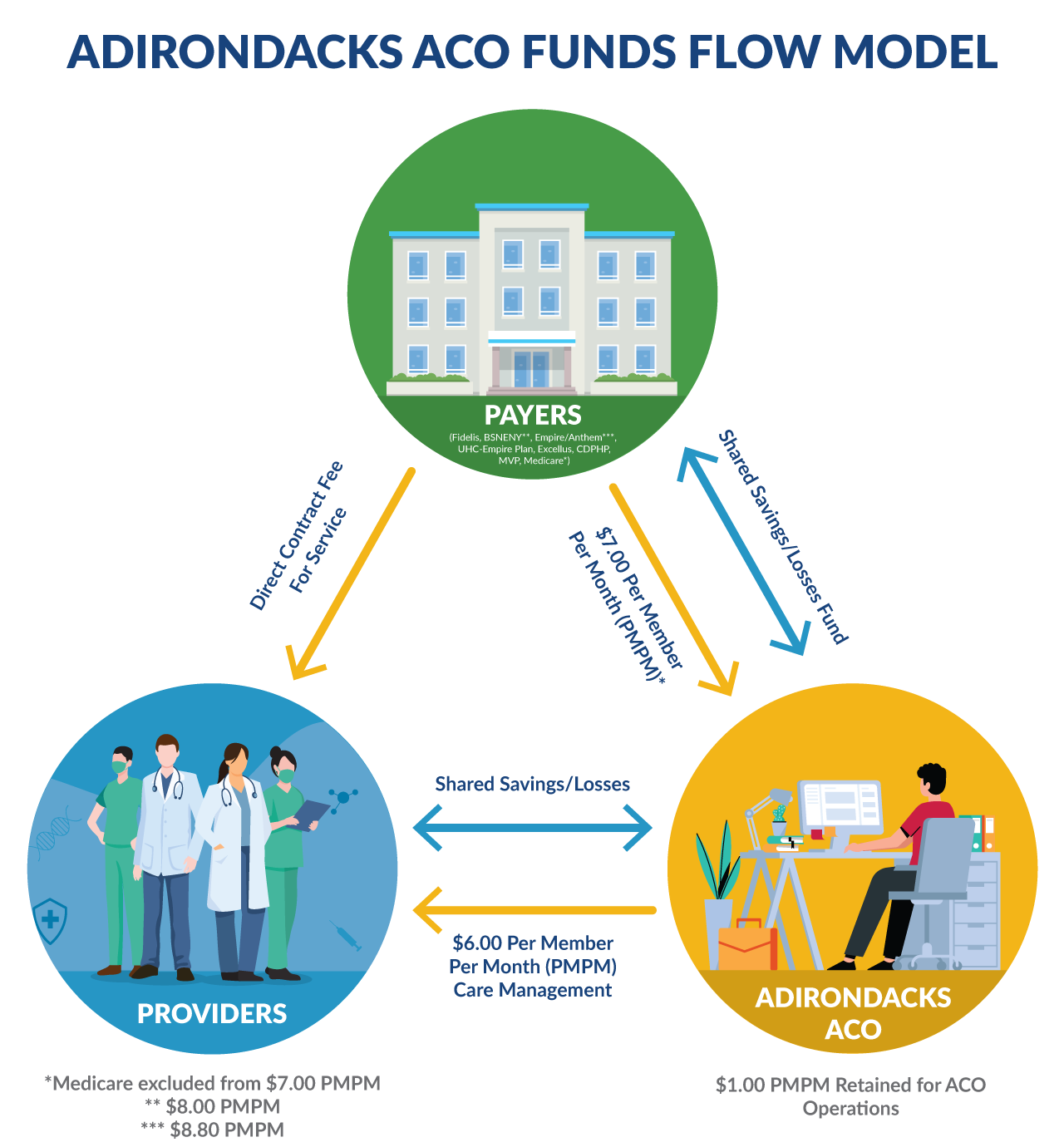
Financial: Adirondacks ACO Funds Flow
The Adirondacks ACO continues to ensure that the Per Member Per Month (PMPM) funds flow to our participating primary care providers on behalf of our payer partners. The ACO administrative costs continue to be carefully monitored to ensure that only a fraction of the total PMPM is needed to support our infrastructure.

Financial
Maximize provider incentives while mitigating downside risk

Quality & Data
Align metrics and data reporting across all payers and reduce the administrative burden for each provider organization

Network & Community
Maximize attribution and expand support for Community Based Organizations that enhance our Mental Health and Substance Use Disorder/Primary Care Provider Integration
1115 Waiver – Social Care Network
1115 Waiver
Adirondack Health Institute, in collaboration with the Fort Drum Regional Health Planning Organization and Northwinds Integrated Health Network, applied to the NYS Department of Health Office of Health Insurance Programs to be the lead Social Care Network for the state’s 1115 Medicaid Waiver. An “1115 Waiver” gives states flexibility to improve and refine programs to better serve their Medicaid populations. The new amendment period is for 3+ years, formally beginning in April 2024 and ending on March 31, 2027, when New York will need to pursue an extension of the waiver.
AHI has consistently engaged CBOs, primary care providers, behavioral health specialists, substance use providers, hospitals, and other regional stakeholders to strengthen our communities. This alignment, coordination, and communication is essential to improving health outcomes and lowering costs – all to improve the health and well-being of our North Country residents. Key areas of focus for the Social Care Network include:
- Ensuring greater coordination of social care services for specific populations.
- Creating an improved and more accessible experience for Medicaid members seeking social care services.
- Establishing financial and operational sustainability, that will continue to deliver services after the end of the 1115 waiver amendment period.
- Promoting more equitable delivery of social care services and addressing the health, racial/ethnic, socioeconomic, and geographic disparities in existing access and quality.
How will this impact the Adirondacks ACO network?
The identification of Medicaid members is a critical step towards navigating members to health-related social needs (HRSN) services. AHI will meet the State’s goal to have every Medicaid member screened for HRSN at least annually by adopting a “no wrong door” approach. This approach is person centered, providing universal access to screening and services. This involves evaluating all stakeholders that interact with Medicaid members, including SCN members (i.e., social care CBOs) and other healthcare ecosystem partners (e.g., Medicaid MCOs, clinical, behavioral, and care management providers) for readiness to conduct screenings using the State’s screening criteria.
The waiver and Social Care Network approach to social care service navigation is characterized by collaborative partnerships, efficient workflows, and the use of technology to track and monitor referrals. Through continuous improvement efforts and a commitment to standardization and education, the goal is to ensure that Medicaid members receive timely and appropriate access to social care services in the North Country region.
The State of ACO Data Analytics
Adirondacks ACO Becomes a CMS Qualified Registry
In addition to report development, in 2023 the Data Analytics team applied and received approval for the ACO to be recognized as a CMS Qualified Registry. A Qualified Registry is a Centers for Medicare & Medicaid Services (CMS) approved vendor that is authorized to collect clinical Merit-based Incentive Payment System (MIPS) quality data from clinician groups and report this data to CMS on their behalf for the purposes of meeting the requirements of CMS’ Quality Payment Program.
While the ACO has always had the authority to collect and submit MIPS data on its providers behalf, this new recognition provides strategic opportunities for the ACO’s data team to expand their CMS reporting capabilities.
Adirondacks ACO Data and Performance Tools
State of ACO Data Analytics
In 2023, the Data Analytics team welcomed a new team member, Karlee Strong, and, with a fully staffed team, they shifted their focus from 2022’s implementation of the ACO’s new data system to building a series of foundational reports for the ACO, leveraging the new system. These ACO reports were built in an interactive dashboard style format and are available to authorized users through a web-based reporting portal.
1. Pre-Visit Planning Report (PVPR)
The PVPR replaced the ACO’s Wellness Visit Report. This newest edition, updated monthly, reflects claims and clinical data for patients attributed to a primary care provider based on frequency of services. The PVPR contains separate tabs, listing each primary care organization’s attributed patients who…
- Are due for a wellness visit (including a well-child visit),
- Are due for at least one of four screenings (colorectal, breast, cervical, chlamydia), and/or
- Were diagnosed with a chronic condition in prior years but not within the last year.
2. Daily Admissions and Discharges Report
This new report, refreshed each business day, lists ACO members having at least one of the following encounters in the prior day, the prior seven days, or the prior 12 months:
- emergency department admission,
- inpatient admission, and/or
- inpatient discharge.
This report is available to both the ACO’s Primary Care provider organizations and for the Northwinds IPA partner organizations.

3. Gaps in Care (GIC) 2.1 Report
This report was newly rebuilt in 2023. The GIC provides detailed information on all open patient gaps received from the ACO’s commercial payors. The rebuilt version includes ALL quality measures tracked by ALL of the commercial payors, with the priority measures placed at the beginning of each table. An interim quality measure scorecard was also added to this report, allowing provider organizations to see their current quality measure results in comparison to the overall ACO results and to the commercial benchmarks.
4. Attributed Patient Report
This new report provides a list of those ACO members who have been attributed to each ACO (primary care) provider organization. As with the PVPR, patients are attributed to a primary care provider based on frequency of services, with PCP attribution continuing to be a work in progress. Features of this report, which is updated monthly, include:
- Detailed ACO member information.
- The ability to filter the list by the attributed PCP, the patient, and /or the health plan/payor.
5. QUIC 2.1 Dashboard
This dashboard was originally developed in 2021 for our Northwinds IPA partners to assist them in achieving the goals of their Medicaid Managed Care and HARP value-based contracts. In 2023, the dashboard was entirely redeveloped and redesigned. This renovation expanded the number of represented Northwinds partner organizations by incorporating additional encounter data for attribution, expanded claims data from one health plan to six health plans, brought in Hixny clinical data to supplement the claims data, added three quality measures, and shifted to a more frequent, monthly refresh cycle.
6. Diabetes Dashboard
This new dashboard was developed for the ACO’s Diabetes Initiative, a workgroup of the ACO’s Population Health Advisory Committee. This dashboard includes ACO population specific information on 1) the prevalence of diabetes and pre-diabetes, 2) the rates of diabetic control and diabetes-specific care, and 3) the utilization of emergency and inpatient acute care by diabetics and pre-diabetics as compared to those without these conditions. The dashboard is updated monthly to allow the workgroup to identify trends and to better focus quality improvement efforts.
Citizenship Criteria: 2023 Performance Year
2023
Citizenship Summary Preview
- ACO: 94% of all ACO providers achieved a score of 100% across all criteria (8 total points).
- ACO providers improved scores on care coordination (94% achieved on average in 2023 vs. 78% in 2022) and engagement (100% achieved in 2023 vs. 85% in 2022).
- 100% of all ACO and Northwinds providers met the citizenship criteria for engagement!
- Northwinds: 92% of all Northwinds providers achieved a score of 100% across all criteria (8 total points).
- Northwinds providers greatly improved scores on care coordination and quality (93% achieved on average in 2023 vs. 44% in 2021 – massive improvement!)
2024 Citizenship Updates
Small changes have been implemented for ACO practices in 2024:
- Quality – Clarification on supplemental data due dates for submission, by payer. Outlined that gaps in care (GIC) reports will be made available in the AHI reporting portal at various times throughout the year.
- Care Coordination – Aligned language for risk stratification with NCQA renewal requirements. For reporting on measures, shifted the date range to a full calendar year (1/1/24 – 12/31/24) for ease in pulling data.
- Engagement – For staff, attendance at two separate work groups will be required.
Small changes have been implemented for Northwinds providers in 2024:
- Quality – NWIHN team will engage with providers throughout 2024 on a system wide process improvement plan that will involve increased utilization of the QUIC dashboard.
- Care Coordination – Added a 3rd measure to report on – Follow-Up After ED Visit for Mental Illness or Alcohol/Drug Dependence (7-day) and changed the date range to a full calendar year (1/1/24 – 12/31/24) to ensure ease in reporting.
- Engagement – Requiring a provider to attend one of the two annual ACO Provider meetings, peers will be included as a provider. For staff, attendance at two separate workgroups will be required.
Adirondacks ACO Staff
“Within our ACO team and throughout all of our partner organizations, I am honored to be working alongside such talented, compassionate, and professional individuals. The client focused work as well as the behind the scenes work happening to improve the health and wellbeing of the Adirondack region is incredible.”

Support Specialist II
Adirondacks ACO

Karen Ashline

Jun Chon, M.D.

Sarah Wright

Jeff Hiscox

Jeremy Powers

Laura Morris

Katy Margison
Director of Partner Engagement and Communications

Melissa Joyce
Support Specialist II

Karlee Strong

Kate Pabst

Lisa Cyphers

Tyler Babbie

Amber Guay
Adirondacks ACO
Insurance Plans
Adirondacks ACO serves as the provider network for government-sponsored and commercial insurance plans called “payers” that are available to New York residents. By partnering with an ACO like us, government and commercial payers can offer affordable insurance products where the provider network is motivated to deliver quality care at a lower cost, which benefits the patient, the payer, and the provider.
