Contract & Network Update
The AHI/ACO Hixny Client Data Warehouse – An Overview
What is the AHI/ACO Hixny Client Data Warehouse (CDW)?
The AHI/ACO CDW is a secure, central depository for ACO members’ claims and clinical data that is hosted by Hixny. Ultimately it will provide the ACO with: 1) a more comprehensive view of patients’ service use, 2) a more comprehensive view of patients’ clinical statuses, and 3) self-analytics capabilities.
How does it work?
The journey of a patient encounter from the provider’s office into the CDW involves a five-step process (see corresponding image below):
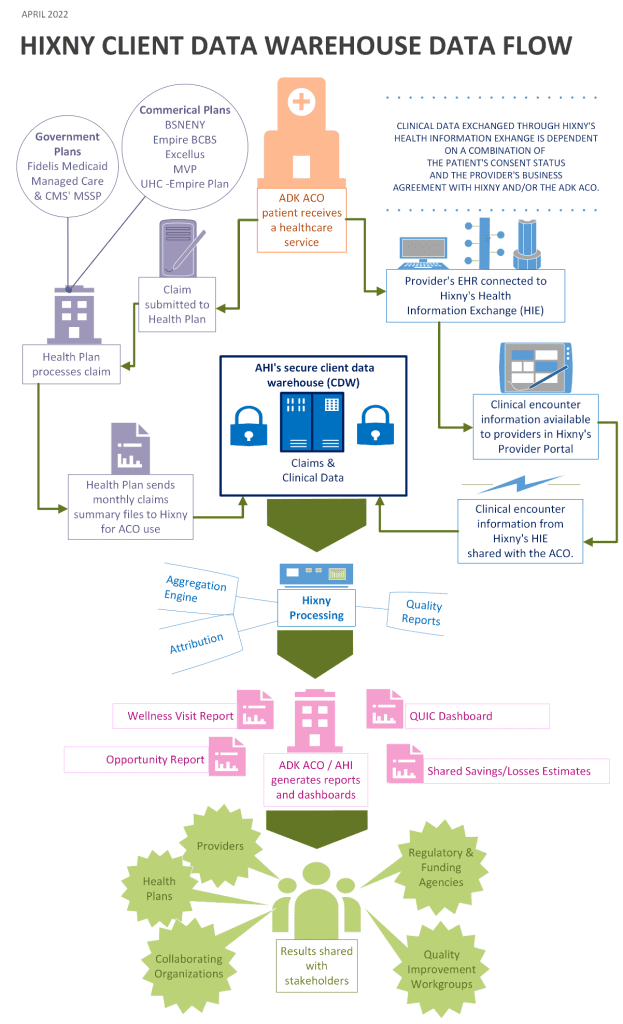
- The flow of information starts when an ACO patient receiving a service (anywhere). At this point two things happen: 1) Clinical data is captured in the provider’s EHR, and 2) a claim is generated and submitted to the patient’s health plan.
- The encounter information is then processed as follows:
- The claim is processed by the health plan and then the plan sends a monthly patient-level claims summary file to Hixny for inclusion in the CDW.
- At the same time, the clinical data flows from the provider’s EHR into the Hixny Health Information Exchange (for participating providers) and is then 1) made available to the provider in their provider portal, and 2) specific clinical information flows in the CDW.
- Hixny then processes the data in order to accurately and consistently bring the information into the CDW.
- The analysts will then be able to work their magic on the compiled encounter data. Once fully implemented, all of the reports and analyses that you’re already familiar with will reflect all of the data available in the CDW (claims and clinical).Plus, new types of reports and analyses can be developed.
- The last step is to share the generated analyses/reports with the ACO’s stakeholders – that’s not only the providers but also stakeholders such as payers, quality workgroups (such as the Diabetes Program), collaborating CBOs, and many others.
When we start to see the impact of the CDW on reporting?
Due to the technical complexity of this project, the implementation of the CDW is a marathon and not a sprint. The negotiations with Hixny started nearly a year ago. While progress has been steady, we do not expect all of the claims data to be fully integrated into the CDW until the end of 2022. In the meantime, the ACO/AHI analysts are working with Hixny to develop pre-built reports, as well as to learn how to build their own ad hoc reports in the new system.
MSSP ACO Beneficiary Notification Requirements
The 2018 Medicare Shared Savings Program Final rule (425.12) acknowledged the requirements for how ACO Participants would notify beneficiaries of their participation in an ACO shared savings program. This final rule was implemented in performance year 2019 and continues today.
ACO Participants should notify their beneficiaries in the following manner –
- An approved CMS poster should be on display at all times in the ACO participant facilities where beneficiaries receive primary care services.The approved poster template was provided by the ACO and can be found here (add link for poster).
- ACO participants must provide a separate written notification approved by CMS to beneficiaries prior to or at their first primary care visit of each performance year.The approved CMS template was provided by the ACO and can be found here (add link for notification)
- ACO participants are encouraged to distribute the notice to beneficiaries at the point of care in order to address any beneficiary questions or concerns; however, they are permitted to distribute beneficiary notifications through electronic transmission (such as email or secure portal) or mail. Regardless of the method used, the ACO participant must maintain and make available evidence that a notification was distributed to each beneficiary.
If you have any questions regarding this required notification, please reach out to Karen Ashline at kashline@cvph.org.
DOWNLOAD CMS Beneficiary Information Notice Here
DOWNLOAD CMS Poter Template Here
Meg Henning joined the Adirondacks ACO Team in 2019, previously working for OneCare Vermont. She is a valuable member of our support team and is eager to focus her efforts, to ensure that the many ACO project tasks are completed in a timely manner. Meg is persistent, but gentle with reminders and has an optimistic view to almost any challenge. Her previous experiences in digital marketing, consumer analysis, data analysis, and even time spent in the fashion industry gives her unique perspectives on community and provider outreach.
Over the past several months she developed the ACO Annual report in an online version and has continued to develop and expand our website presence. She has committed herself to the consistent growth and expansion of skills required of her, with the goal set on innovation and success of the ACO.
In her off time, Meg is a devoted mother of Owyn, her one year old son, who she raises with her husband. Meg lives in Vermont in the small town she grew up in – recently moving to her childhood family home. In their together time, she and her husband are sharing the Vermont way of life with young Owyn and their extended family.
Quality & Performance Update
Depression Screening and Follow-Up Plan Nuances
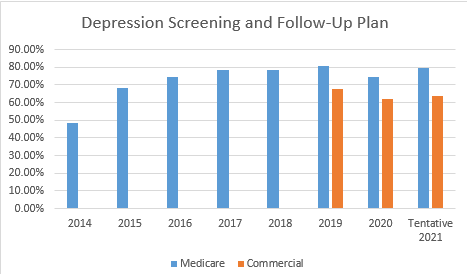
Depression Screening and Follow-Up has been part of our measure sets since 2014 with the Medicare Shared Savings Program and in 2019 part of our Commercial arrangements. Our overall performance has increased with many different variables influencing the results, such as the COVID pandemic for 2020 and 2021. The move to telehealth visits, required significant changes to workflow to incorporate such screenings. The measure has had some significant changes made over the years.
The measure is looking at the percentage of patients aged 12 and older screened for depression on the date of the visit or up to 14 days prior to the date of the visit using an age appropriate standardized tool. If the screening is positive, a follow-up plan is documented on the date of the visit. The intent of the measure is to screen for depression in patients who have never had a diagnosis of depression or bipolar disorder prior to the visit. Patients with no prior diagnosis of depression may use a PHQ-2 for the screening. If there is any history of depression, even if in remission, a PHQ-9 screening must be used.
A positive screen on the date of the visit requires a documented follow up plan. A follow up plan must include one of the following:
- eferral to a practitioner for additional evaluation and assessment to formulate a follow up plan for a positive screen
- Pharmacological intervention
- Other interventions or follow-up for the diagnosis or treatment of depression such as behavioral health evaluation, psychotherapy, pharmacological interventions and additional treatment options
Other tips to remember about this measure:
- The name of the age appropriate standardized depression-screening tool must be documented in the medical record.
- The patient must be screened once during the measurement year, if more than one completed use most recent screening for depression.
- The eligible professional needs to make the determination whether the screening is positive or negative.
- Screening for depression may be completed during a telehealth encounter along with the documentation of a follow up plan if screening is positive.
There are several opportunities to improve the overall capture rates for depression screening:
- Partner with HIXNY to ensure the clinical data being sent is captured and reflected correctly
- Partner with your EMR vendor to look at the workflow established is capturing the data appropriately
- Educate your staff around the nuances of the appropriate tool to utilize when screening a patient
As always, thank you for all you do each day for our patients and our communities.
